-
09 July 2020

 As a hospice nurse at Federation partner agency JSSA, Stephanie Simenauer Lynn has something of an ideal standard and a perfect vision for how she and her team administer end-of-life care for their patients. She wants to help them achieve a “gentle landing,” a calm and tranquil death, without physical suffering and with loved ones by their side.
As a hospice nurse at Federation partner agency JSSA, Stephanie Simenauer Lynn has something of an ideal standard and a perfect vision for how she and her team administer end-of-life care for their patients. She wants to help them achieve a “gentle landing,” a calm and tranquil death, without physical suffering and with loved ones by their side.
Most people are drawn to hospice work because of their own experiences, Stephanie believes. Her professional motives, however, are powered just as much by family history as by her personal memories.
“I am the daughter of two Holocaust survivors, and I think that informs how rewarding I find this work,” Stephanie says. Yes, she feels fortunate that her parents were able to live until a “ripe old age” until they died under the care of JSSA hospice. But she is also driven “to help Jews in particular have a dignified and peaceful death that so many of my extended family were denied in the war.”
Of course, the coronavirus pandemic is vastly different from World War II. But similar to how the Holocaust deprived so many of a dignified death, our community’s current crisis has made it more difficult for Stephanie and her team to provide the end-of-life experience they want for patients and their families.
When interviewed in May, Stephanie noted, “We feel like we can’t do our best work [right now. We’re seeing patients in much more stressful circumstances.”
Stephanie, who is responsible for the initial visit to enroll a patient in hospice care, does most of her work in facilities—like nursing homes, assisted-living centers, and group homes—that have been short-staffed and overtaxed during the pandemic.
Not only are more people getting sick, but those who enter hospice are also dying more quickly than they had before. According to Stephanie, the average length of stay for a hospice patient is typically around two weeks; but for those infected with coronavirus, the average is approximately two days. Under those conditions, it’s difficult to get to know the family and provide that “gentle landing” for the patient.
In addition, family members have not been allowed to enter these facilities since mid-March, so they cannot physically be with their loved one when they die. “It was more family-oriented prior to the coronavirus,” Stephanie says of her work.
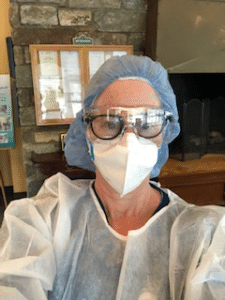 Without the presence of family, Stephanie would prefer to provide as much comfort as she can to her patients—but even that is difficult right now. While she is grateful to have access to essential personal protective equipment (PPE), including a gown, gloves, N95 mask, and a pair of goggles or a safety shield, “the PPE is a barrier between me and the patient,” she says. “I’m used to holding my patient’s hand. Holding hands through a glove doesn’t feel the same.”
Without the presence of family, Stephanie would prefer to provide as much comfort as she can to her patients—but even that is difficult right now. While she is grateful to have access to essential personal protective equipment (PPE), including a gown, gloves, N95 mask, and a pair of goggles or a safety shield, “the PPE is a barrier between me and the patient,” she says. “I’m used to holding my patient’s hand. Holding hands through a glove doesn’t feel the same.”
Of course, Stephanie has concerns for her own safety. But still, she is thankful to be doing her work during this time.
“When you’re in the room with the patient, you have a human being in the bed, and they need care. When you focus on that, the fear does dissipate. You’re focused on doing your job,” Stephanie says. “The importance of the work we do has really been underscored [during the pandemic].”
Especially since family members can’t be in the room, Stephanie says they are extremely appreciative that someone else is there to care for their loved one. As much as she can, Stephanie calls the patient’s children or siblings to give them a report. She tries to arrange a video visit so the family can see their mother or father, brother or sister, aunt, or uncle. At a time when the facility staff might be too busy to communicate regularly with each family, the hospice team does as much as possible to make the family feel a connection to their loved one during these final days.
“We can’t heal their bodies. But there’s an awful lot of other healing that can be achieved,” she says—both for the patient and the family members. In the midst of these most difficult moments, Stephanie maintains there is always some good to be had.
Even under these circumstances, Stephanie still finds her work caring for those who are dying to be incredibly life-affirming. “Family members are so grateful, and that’s what keeps you going,” she says. “You see people who are at their best, even at some of the worst times of their lives. I find that inspiring.”
Thankfully, as of June, the number of coronavirus cases in JSSA hospice care has declined. But with the increased rate of death in Greater Washington during the pandemic, Stephanie has seen a rise in the need—and the importance—of hospice care.
“With the increasing morbidity and mortality in [our community] right now, it seems to me that it’s more essential than ever. People need that kind of support. All deaths are sad. But we can make it less traumatic,” Stephanie says. “I feel pride in the work that I’m doing, and I’m immensely proud of the work that JSSA is doing in this pandemic. I’m proud to be a part of it.”
The Jewish Federation is proud to partner with JSSA to meet the needs of community members across Greater Washington. Along with a network of local human service organizations, Federation and JSSA have launched 703-J-CARING: The Jewish Community Support Line to connect residents in DC, MD, and Northern Virginia to with a case manager who can help callers find resources right for them. As our community continues to weather the coronavirus pandemic and its ensuing challenges, the support of donors to Federation’s Annual Campaign ensures that our human service agencies and other partner organizations are equipped to meet the needs of those they serve—and to be agile in their work during this time of crisis.
